About Shoulder MRI
For shoulder MRI there is no special preparation needed unless you doctor specifically requests it.
- The patient is positioned laying on their back with the injured arm alongside the body and the thumb pointing up, inside the MRI machine or scanner.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the shoulder. This helps to get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
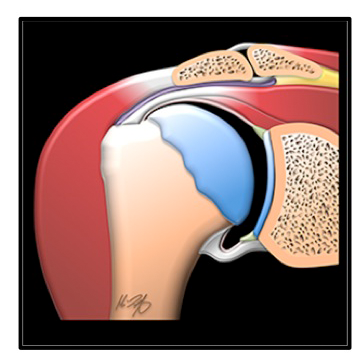
What is MRI used for in the shoulder ?
- MRI allows us to see many of the different structures in the shoulder.
- Several injuries or diseases affecting those structures can be diagnosed using MRI.
- Common things include labral tears or degeneration, damage to the joint capsule, tendons or ligaments that contribute to shoulder stabilization, osteoarthritis, tumors, among others.
.png)
.png)
MRI examinations showing normal shoulder (top) and a rotator cuff tear and bursitis (bottom).
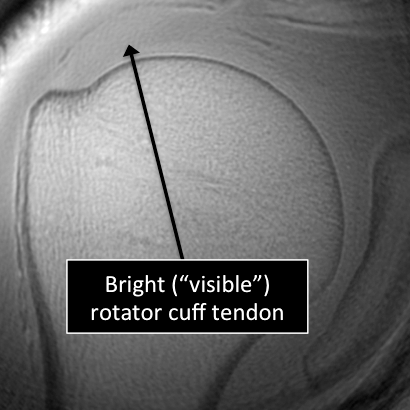
Why Translational MRI of the Shoulder
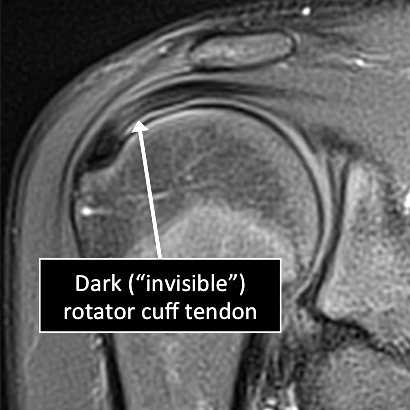
- In the shoulder, as in many other parts of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- Some of these “invisible” or dark structures are unique to the shoulder (glenoid labrum) and others are found in other parts of the body (e.g. cartilage, ligaments, tendons, cortical bone).
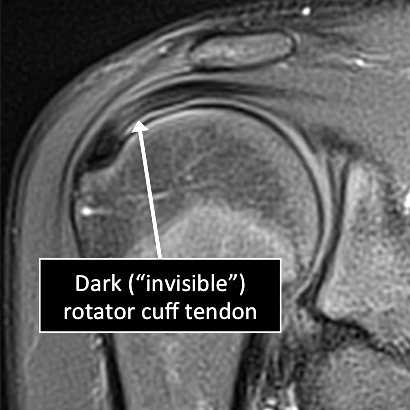
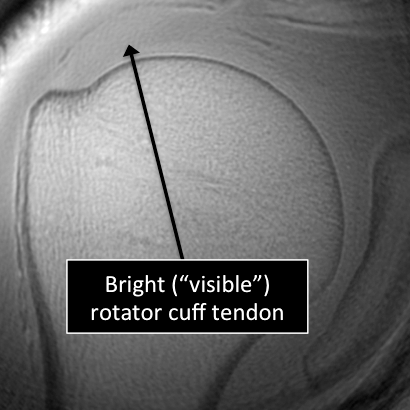
MRI examinations using the standasrd MRI technique (top) and translational MRI technique (bottom).
About Elbow MRI
- For elbow MRI there is no special preparation needed unless your doctor specifically requests it.
- The patient is positioned laying on their back with the injured arm extended alongside the body and the palm facing up, inside the MRI machine or scanner.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the elbow. This helps to get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
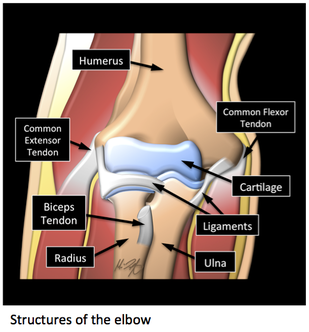
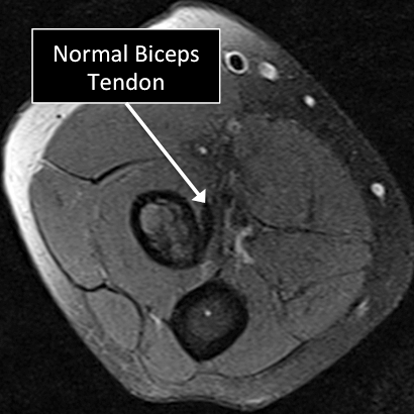
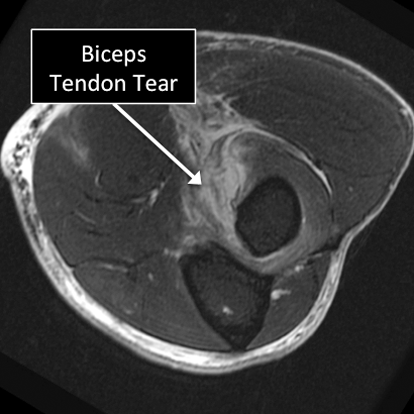
What is MRI used for in the Elbow ?
- MRI allows us to see many of the different structures in the elbow.
- Several injuries or diseases affecting those structures can be diagnosed using MRI.
- Common things include degeneration, partial or complete tears of ligaments and/or tendons, damage to the joint capsule, cartilage defects, osteoarthritis, tumors, among others.
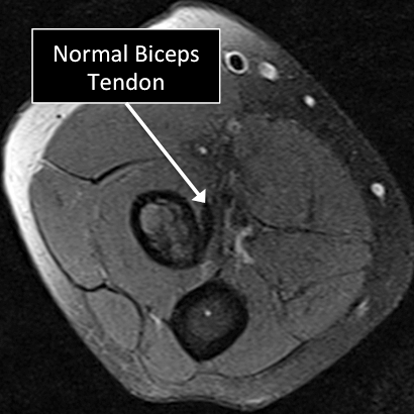
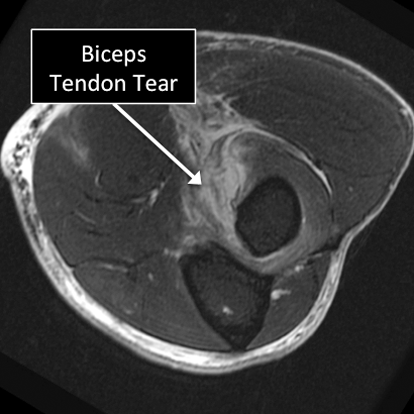
Elbow MRI examinations showing normal (top) and abnormal (bottom) biceps tendon.
Why Translational MRI of the Elbow?
- In the elbow, as in many other parts of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- Some of these “invisible” or dark structures can be found in the elbow and in other parts of the body (e.g. cartilage, ligaments, tendons, cortical bone).
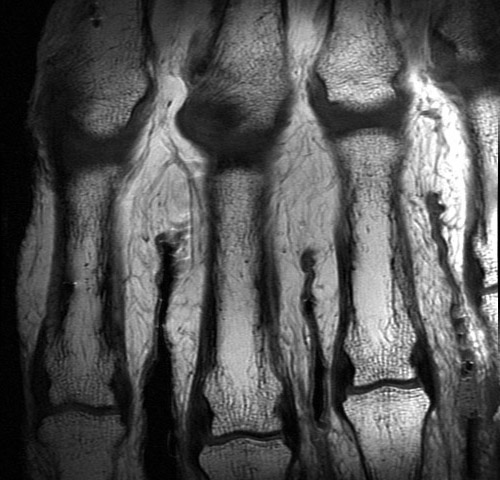
About MRI evaluation of the cartilage
- The cartilage will be assessed when evaluating a MRI of a specific body region.
- For MRI of the musculoskeletal system generally there is no special preparation needed unless you doctor specifically requests it.
- The position of the patient in the MRI machine or scanner will depend on the region of the body to be imaged.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the region to be imaged. This helps to get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
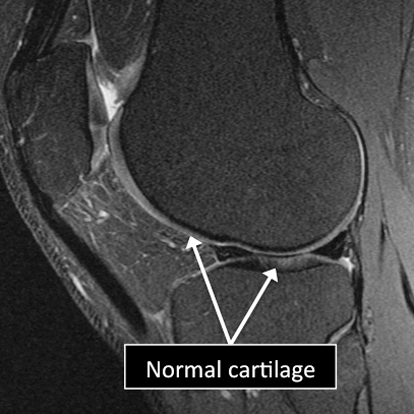
What is MRI used for in the cartilage ?
- MRI allows us to see different regions of the cartilage.
- Several injuries or diseases affecting the cartilage can be diagnosed using MRI.
- Common things affecting the cartilage include degenerative or traumatic defects, abnormal calcium deposition in the cartilage, fractures affecting the cartilage and the underlying bone (osteochondral fractures), among others.
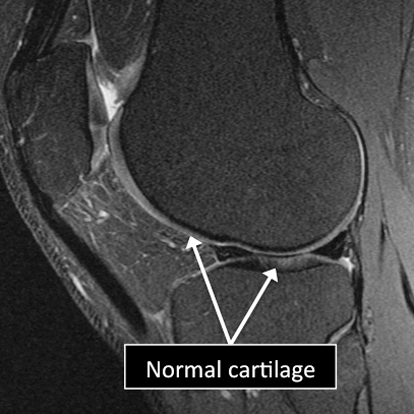
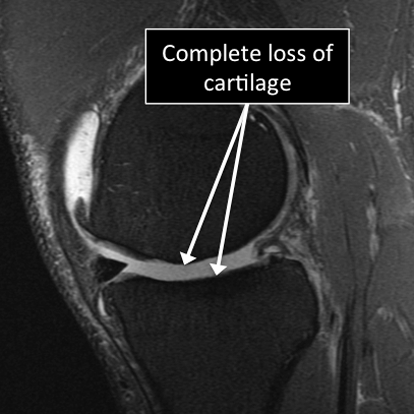
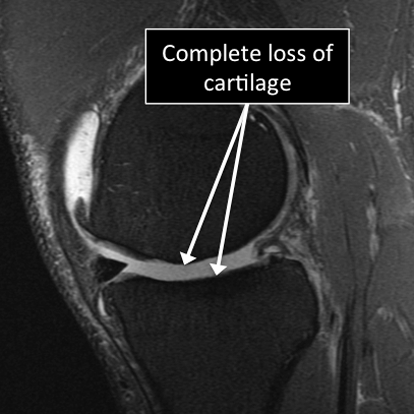
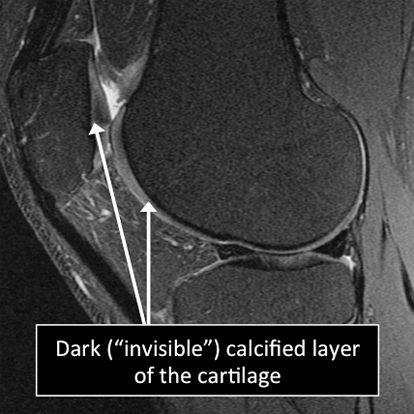
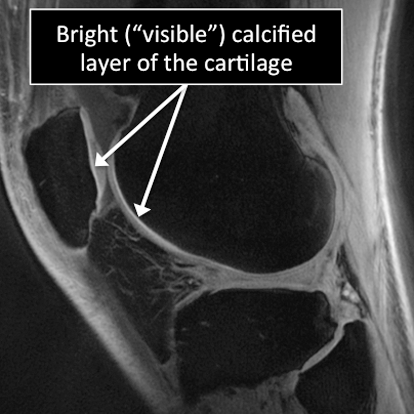
Knee MRI examinations showing normal (top) and abnormal (bottom) articular cartilage.
Why Translational MRI of the cartilage?
- In the cartilage, as in many other tissues of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- In the cartilage these “invisible” or dark structures include the calcified layer and the radial or deep zone of the cartilage.
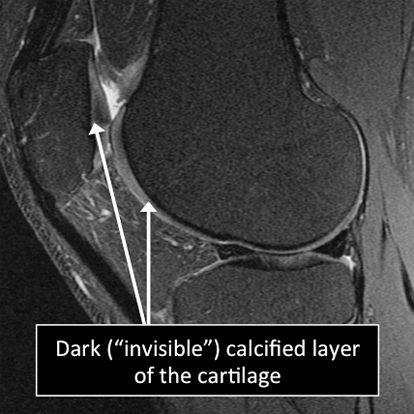
Knee MRI examinations using the standarad MRI techniques (top) and translational MRI techniques (bottom).
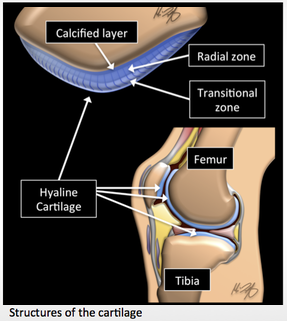
About the hip MRI
- For hip MRI there is no special preparation needed unless your doctor specifically requests it.
- The patient is positioned laying on their back inside the MRI machine or scanner.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the hip. This helps to get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
What is MRI used for in the hip ?
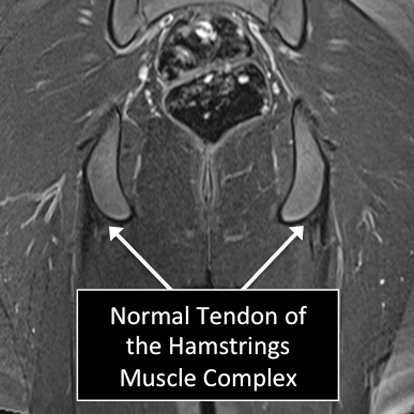
- MRI allows us to see many of the different structures in the hip.
- Several injuries or diseases affecting those structures can be diagnosed using MRI.
- Common things include degeneration, partial or complete tears of ligaments and/or tendons, damage to the joint capsule, labral tears, cartilage defects, osteoarthritis, tumors, fractures, avascular necrosis, among others.
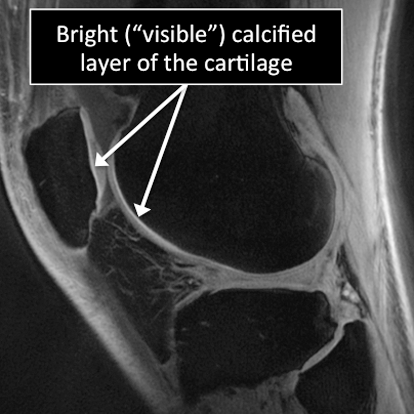
.png)
Hip MRI examinations showing normal (top) and abnormal (bottom) tendon of the Hamstrings Muscle Complex.
Why Translational MRI of the hip?
- In the hip, as in many other parts of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- Some of these “invisible” or dark structures are unique to the hip (acetabular labrum) and others are found in other parts of the body (e.g. cartilage, ligaments, tendons, cortical bone).
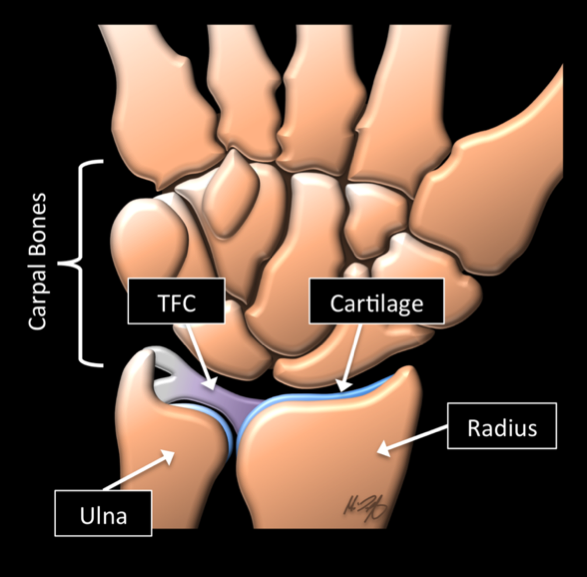
About the wrist MRI
- For wrist MRI there is no special preparation needed unless you doctor specifically requests it.
- The patient lays inside the MRI machine on their back with the arm to be imaged extended alongside the body or on their stomach with the arm extender over the head.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the shoulder. This helps to get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
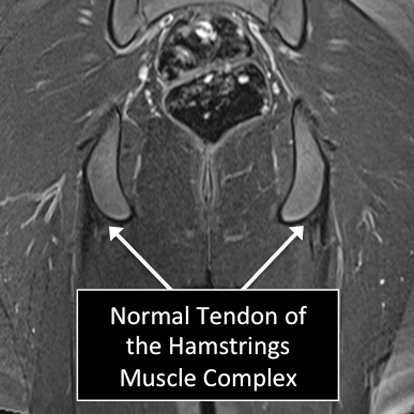
What is MRI used for in the wrist ?
- MRI allows us to see many of the different structures in the wrist.
- Many injuries or diseases affecting those structures can be diagnosed using MRI.
- Common things include fractures (broken bone), ligament and tendon tears, damage to the Triangular Fibrocartilage of the wrist (perforations and degeneration), osteoarthritis, tumors, among others.
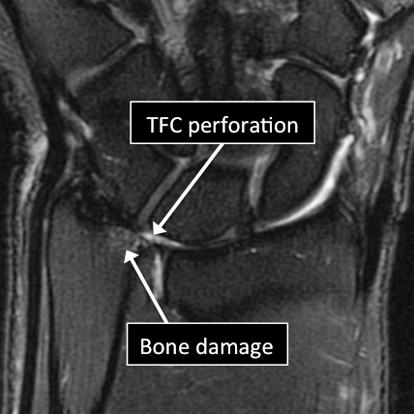
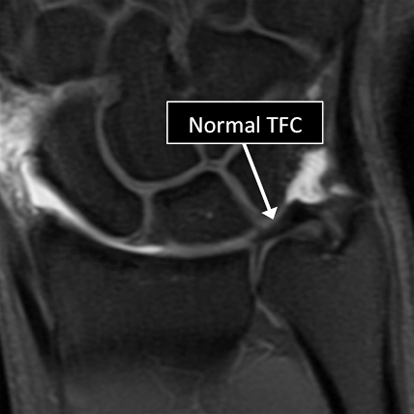
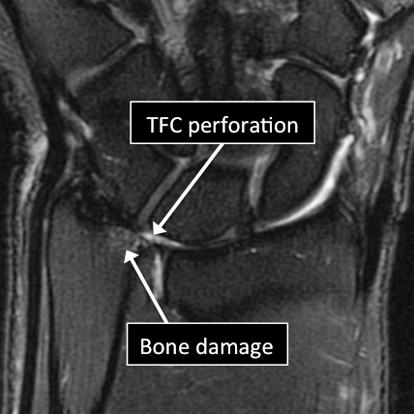
Wrist MRI examinations showing normal (top) and abnormal (bottom) TFC.
Why Translational MRI of the wrist?
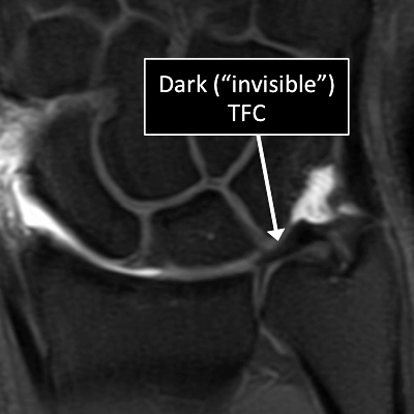
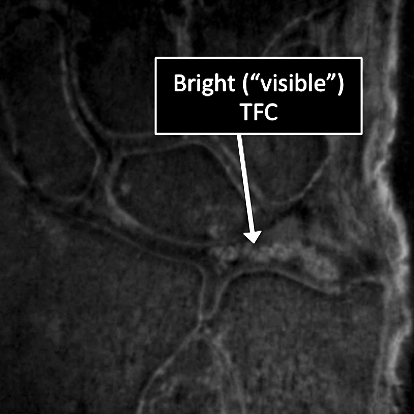
- In the wrist, as in many other parts of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- Some of these “invisible” or dark structures are unique to the wrist (Triangular Fibrocartilage or TFC) and others are found in other parts of the body (e.g. cartilage, tendons, ligaments, cortical bone).
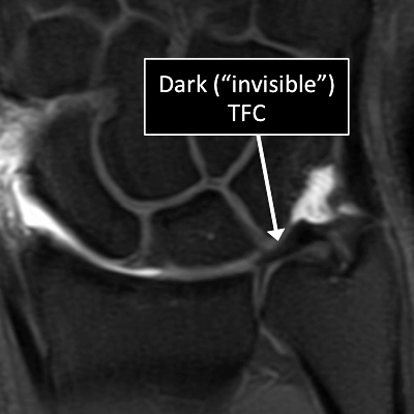
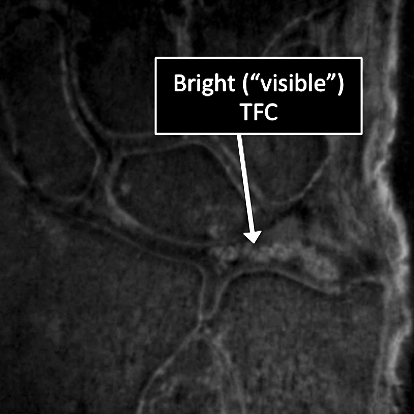
Wrist MRI examinations using the standard MRI techniques (top) and translational MRI techniques (bottom).
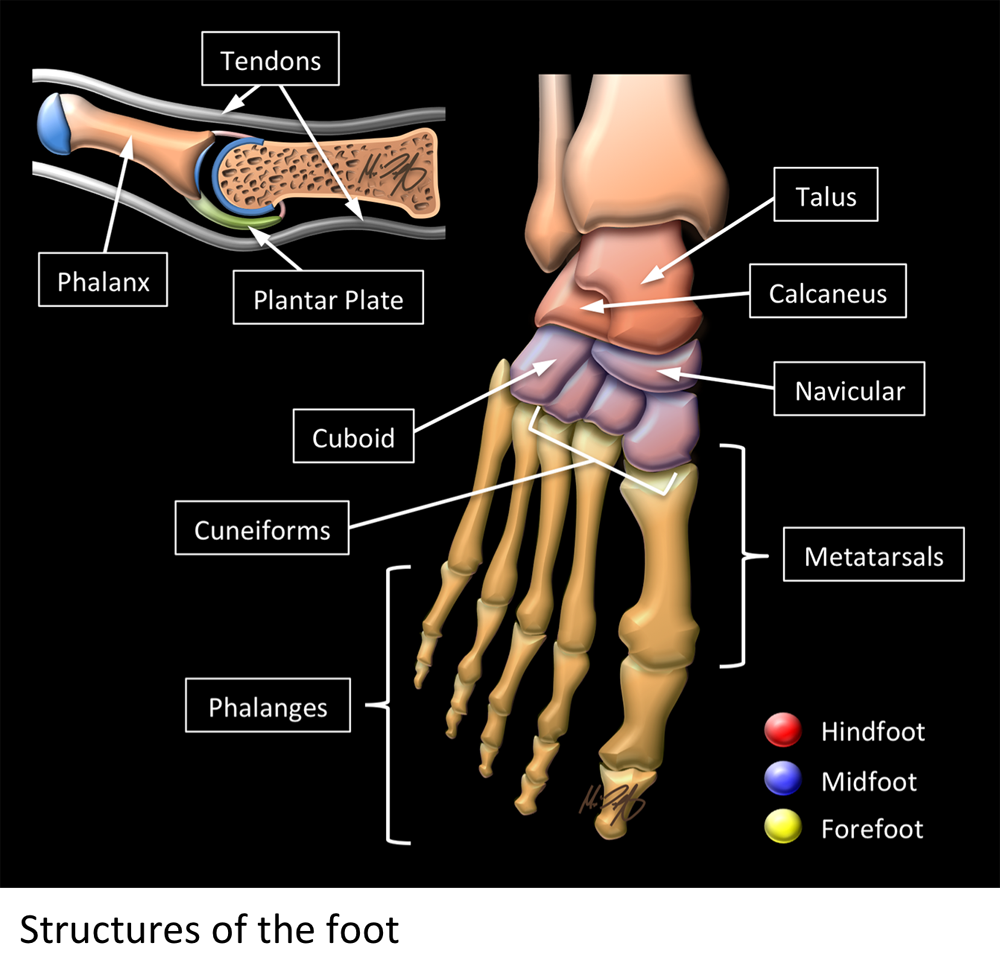
About the foot MRI
- For foot MRI there is no special preparation needed unless your doctor specifically requests it.
- The patient is positioned laying on their back inside the MRI machine or scanner with the foot at right angles to the lower leg.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the foot. This helps to maintain optimal position and get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
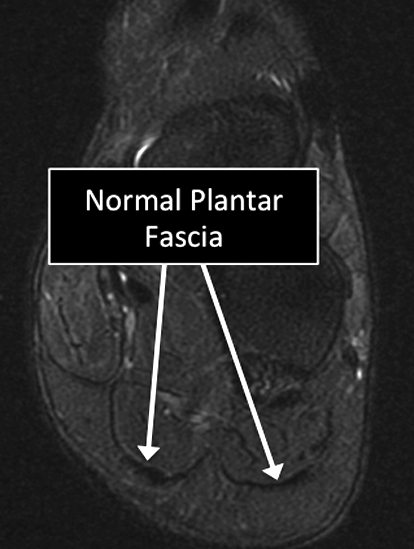
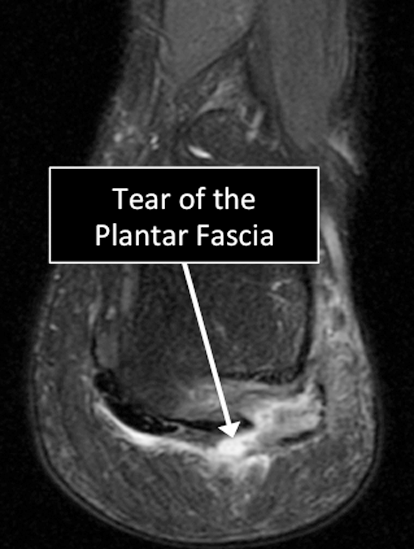
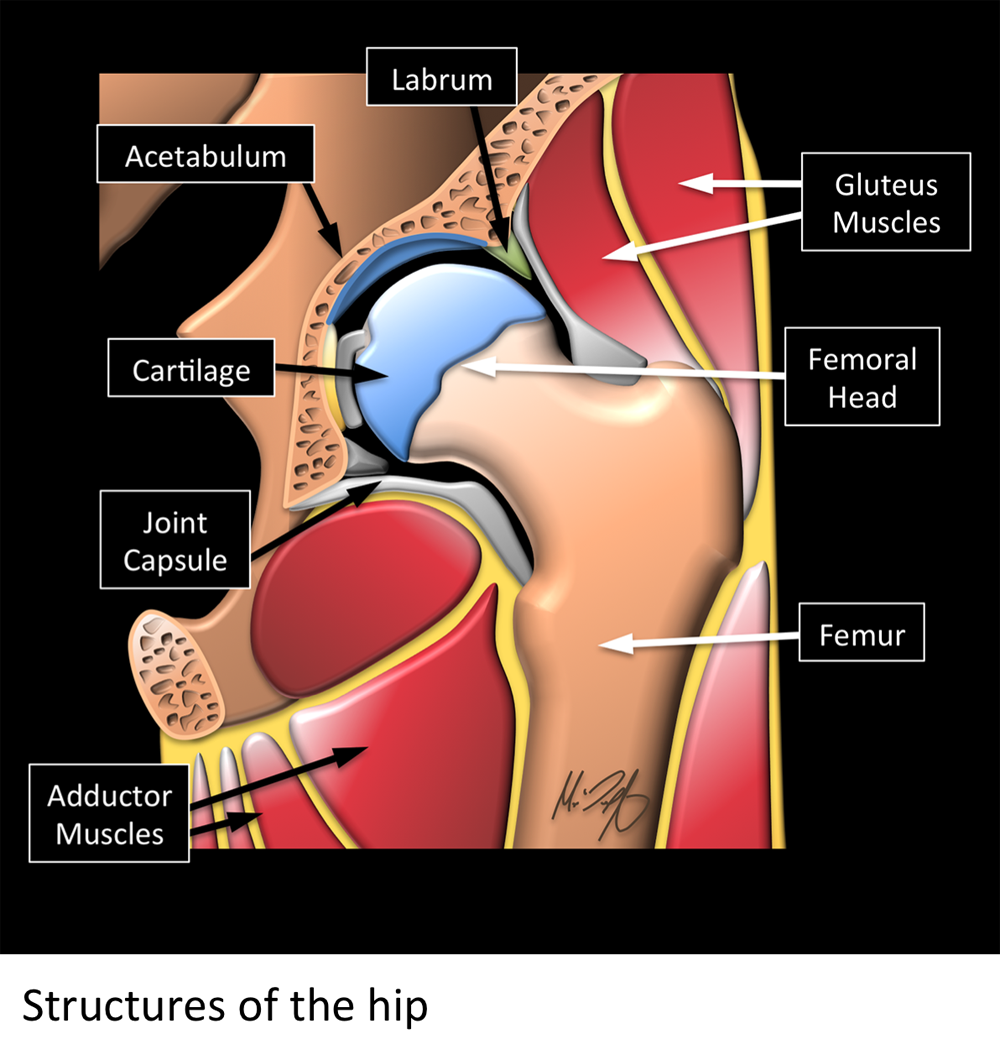
What is MRI used for in the foot ?
- MRI allows us to see many of the different structures in the foot.
- Several injuries or diseases affecting those structures can be diagnosed using MRI.
- Common things include degeneration, partial or complete tears of ligaments and/or tendons, damage to the cartilage and/or underlying bone, plantar plate injuries, osteoarthritis, tumors, fractures, among others.
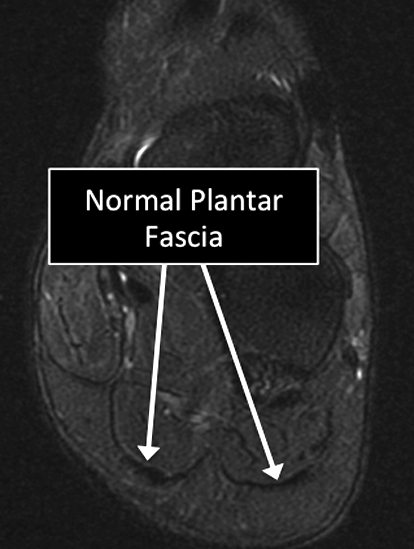
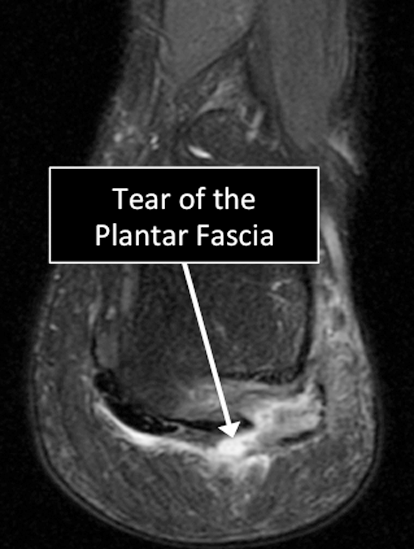
Foot MRI examinations showing normal (top) and abnormal (bottom) Plantar Fascia.
Why Translational MRI of the foot?
- In the foot, as in many other parts of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- Some of these “invisible” or dark structures are unique to the foot (e.g. plantar plates) and others are found in other parts of the body (e.g. cartilage, ligaments, tendons, cortical bone).
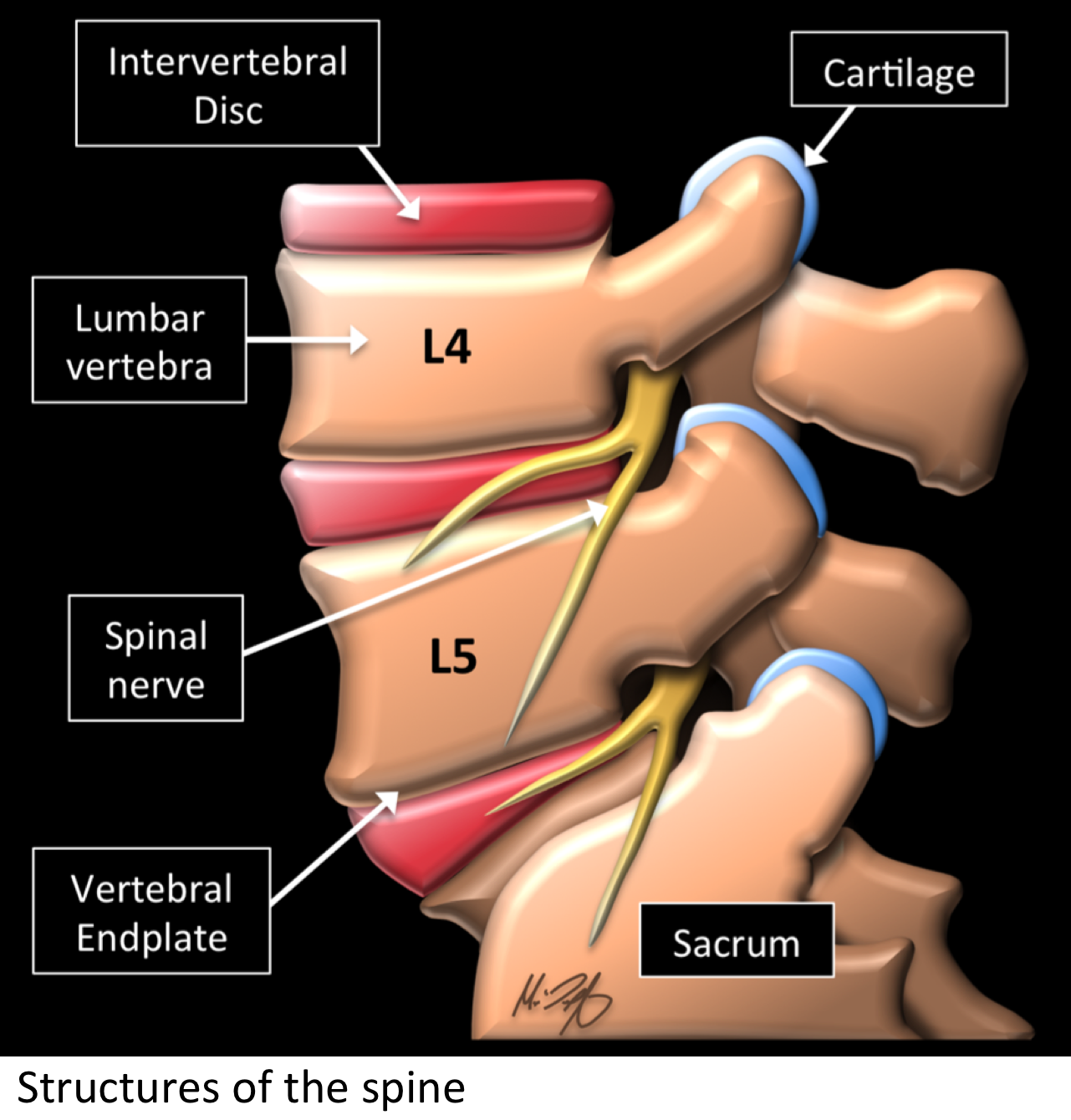
About spine MRI
- For spine MRI there is no special preparation needed unless you doctor specifically requests it.
- The patient is positioned on their back inside the MRI machine or scanner.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the shoulder. This helps to get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
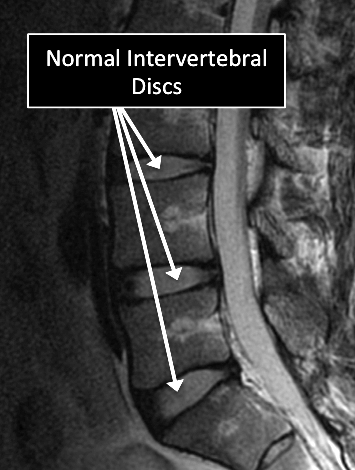
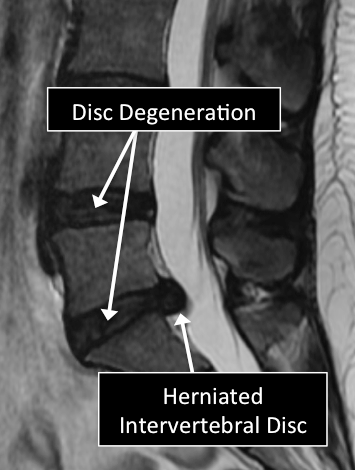
What is MRI used for in the spine ?
- MRI can visualize many of the different structures in the spine.
- Many diseases affecting those structures can be diagnosed using MRI.
- Common injuries and diseases include degeneration and tears of the intervertebral disc (IVD), herniated discs, osteoarthritis, tumors, vertebral fractures, among others.
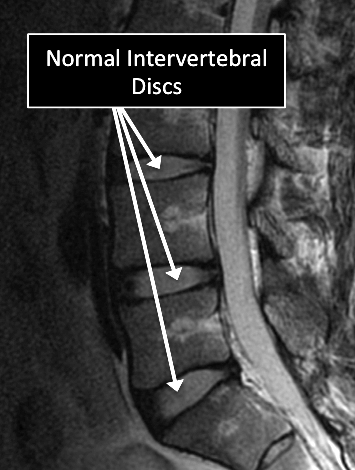
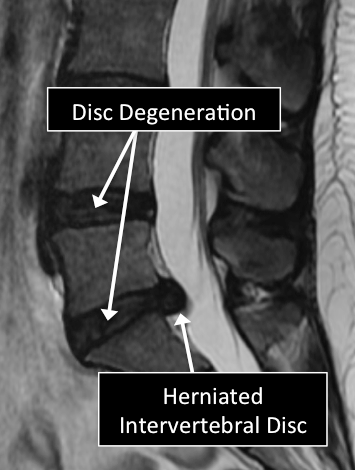
MRI examinations showing normal (top) and abnormal (bottom) lumbar spine.
Why Translational MRI of the wrist?
- In the spine, as in many other parts of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- Some of these “invisible” or dark structures are unique to the spine (vertebral endplate) and others are found in other parts of the body (e.g. ligaments, cortical bone, nerves).


Spine MRI examinations using the standard MRI techniques (top) and translational MRI techniques (bottom).
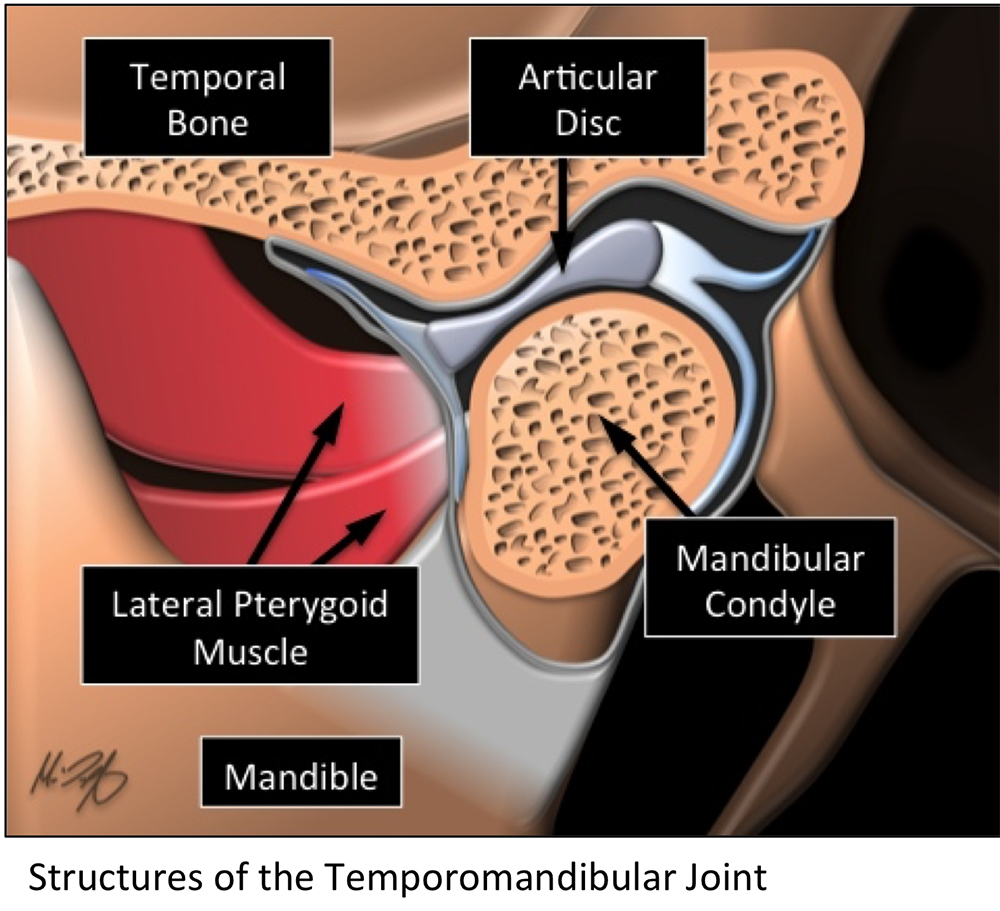
About Temporomandibular joint MRI
For MTJ MRI there is no special preparation needed unless you doctor specifically requests it. As in all MRI examinations, no metallic objects are allowed.
For this study, the patient is positioned laying facing up inside the MRI machine or scanner. The patient is required to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient. The technician will be giving the instructions and will assure that the patient is comfortable during the examination. In the case of the TMJ the patient likely be required to open and close the mouth as directed by the technician or the radiologist.
What is MRI used for in the TMJ?
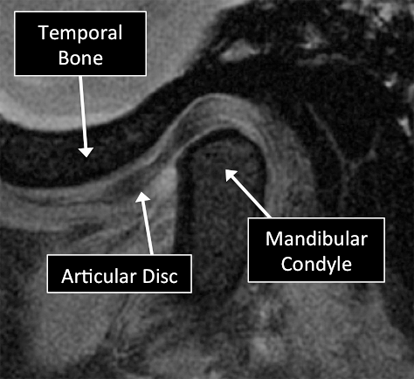
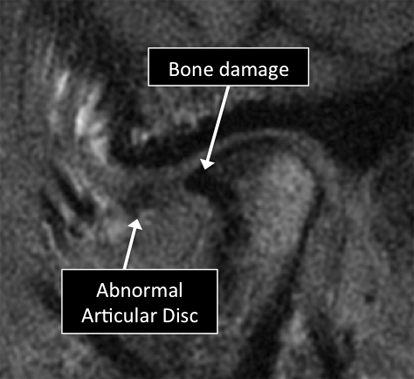
MRI can visualize many of the different structures in the TMJ. Certain diseases affecting those structures can be diagnosed using MRI. Common diseases include abnormal position, tears and degeneration of the articular disc, osteoarthritis, tumors, among others.
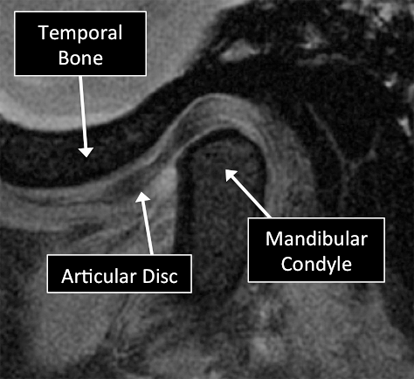
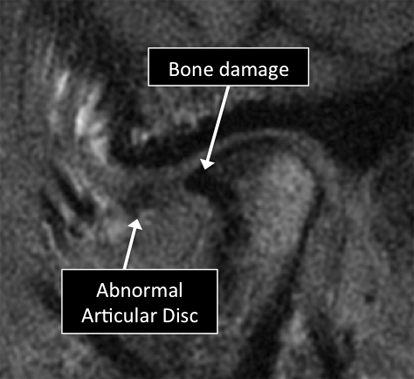
MRI examinations showing normal (top) and abnormal (bottom) TMJ.
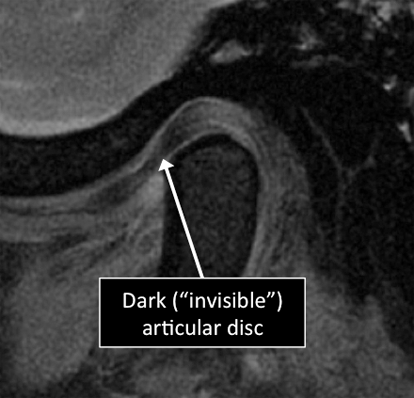
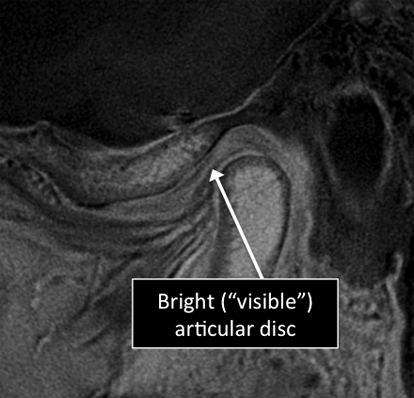
Why Translational MRI of the TMJ?
In the TMJ, as in many other parts of the body there is certain structures that can’t be seen with the standard MRI used in the clinical practice. There are new techniques that allow the visualization of some of the structures which are otherwise “invisible” in the standard MRI. Some of these “invisible” structures are unique to the TMJ (articular disc) and other are found in other parts of the body (e.g. tendons, ligaments, cortical bone).
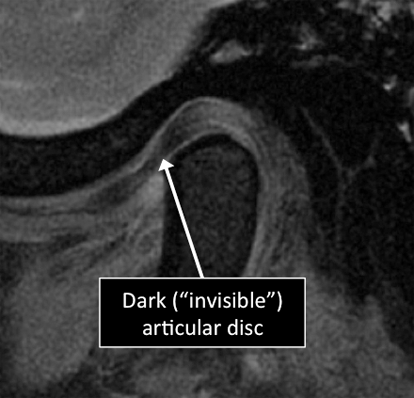
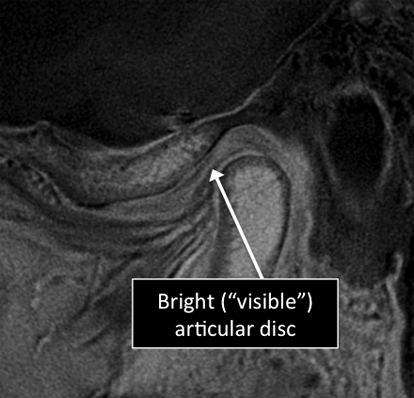
TMJ MRI examinations using the standard MRI techniques (top) and translational MRI techniques (bottom).
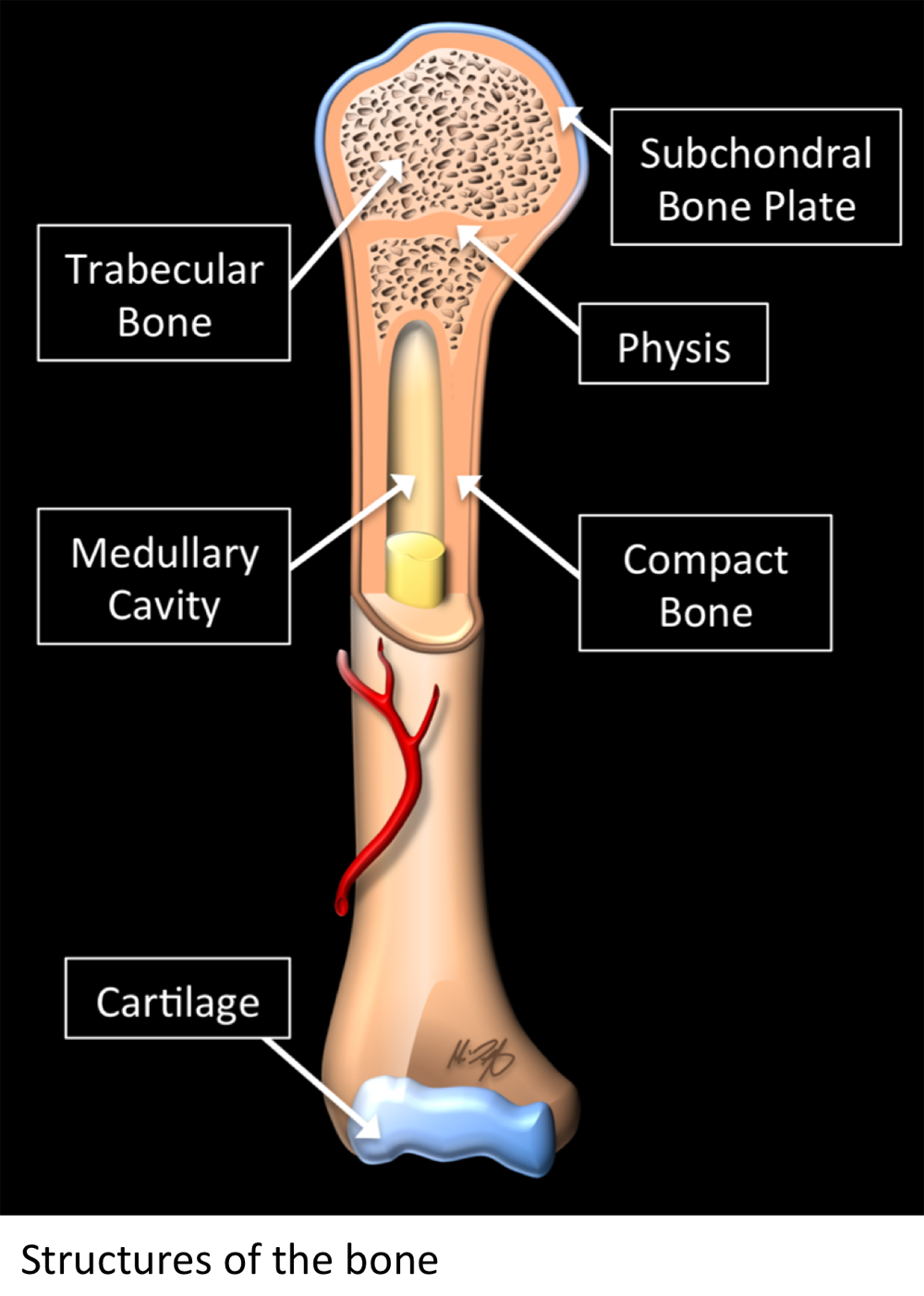
About MRI evaluation of the bone
- The bone will be assessed when evaluating a MRI of a specific body region.
- For MRI of the musculoskeletal system generally there is no special preparation needed unless you doctor specifically requests it.
- The position of the patient in the MRI machine or scanner will depend on the region of the body to be imaged.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the region to be imaged. This helps to get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
What is MRI used for in the bone ?
- MRI allows us to see many of the different structures in the bones.
- Several injuries or diseases affecting those structures can be diagnosed using MRI.
- Common things affecting bones include osteoporosis, tumors, fractures, osteoarthritis, among others.
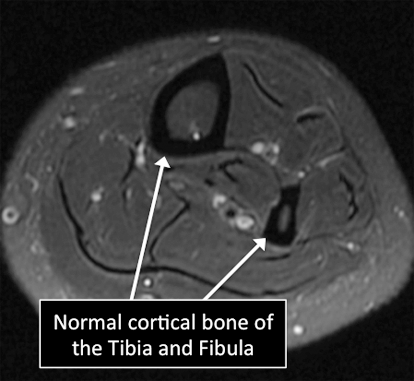
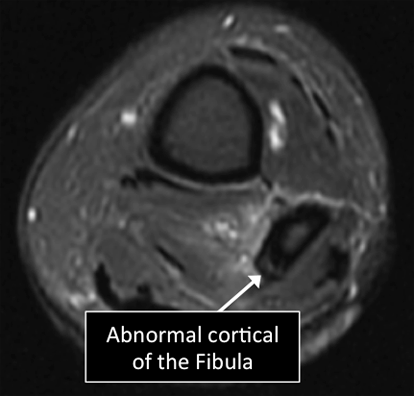
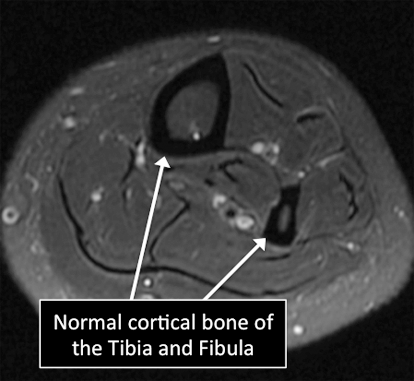
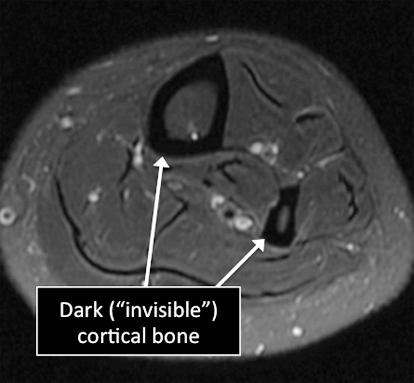
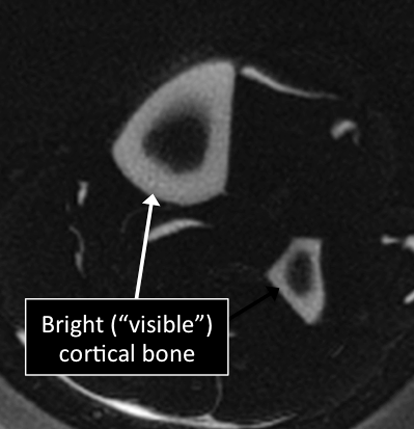
Leg MRI examinations showing normal (top) and abnormal (bottom) cortical bone.
Why Translational MRI of the bone?
- In the bone, as in many other tissues of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- In the bone these “invisible” or dark structures include cortical bone, subchondral bone plate and vertebral endplate.
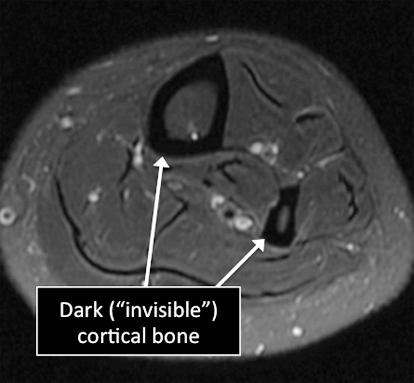
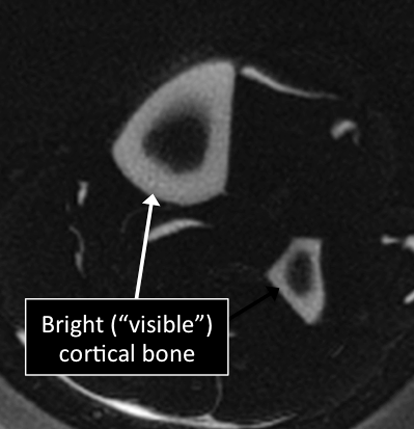
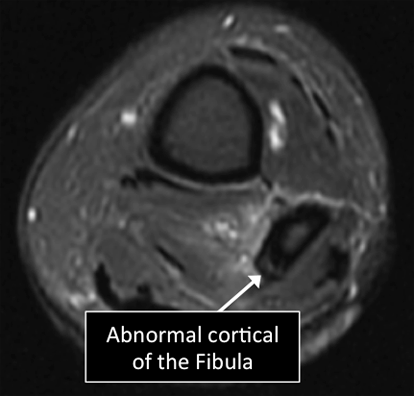
Leg MRI examinations using the standard MRI techniques (top) and translational MRI techniques (bottom).
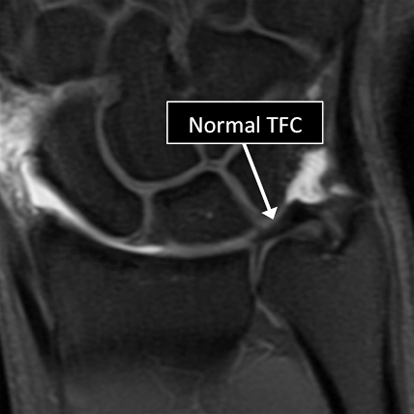
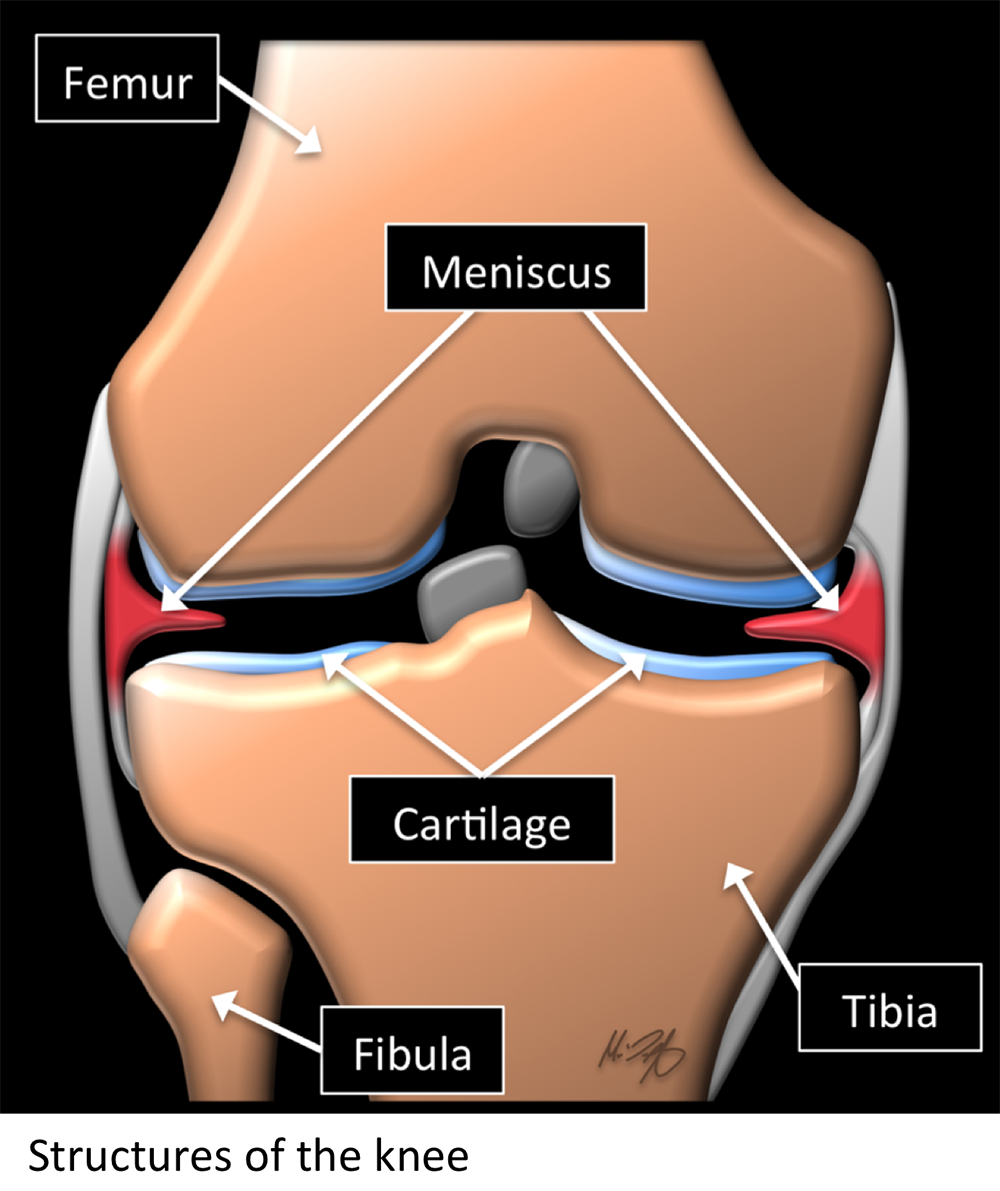
About the knee MRI
-
For knee MRI there is no special preparation needed unless you doctor specifically requests it.
-
The patient is positioned on their back inside the MRI machine or scanner.
-
The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
-
A piece of plastic, called a “coil”, may be placed on the shoulder. This helps to get better quality pictures.
-
The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
What is MRI used for in the knee ?
-
MRI allows us to see many of the different structures in the knee.
-
Many injuries or diseases affecting those structures can be diagnosed using MRI.
-
Common things include meniscal tears, ligament tears or degeneration, osteoarthritis, tumors, among many others.
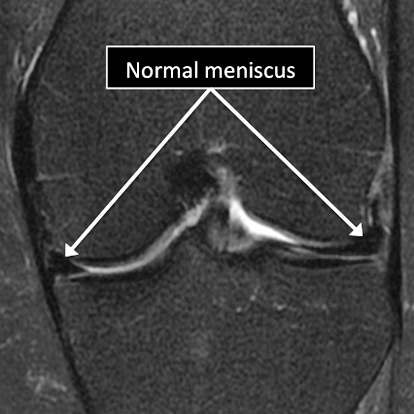
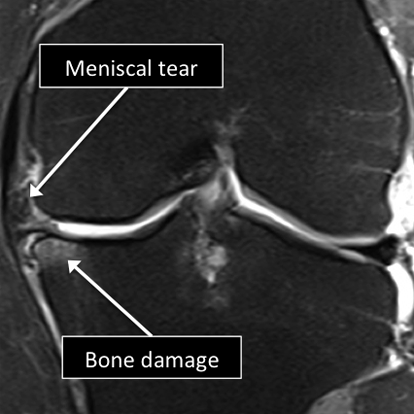
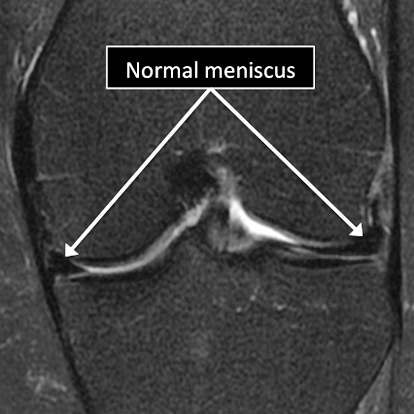
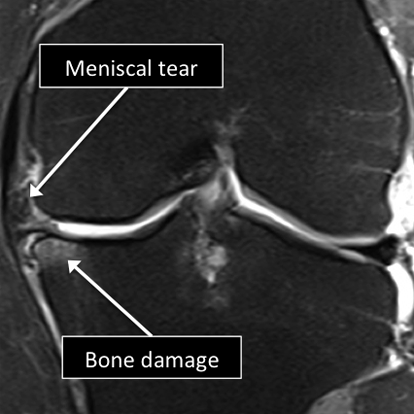
Knee MRI examinations showing normal (top) and abnormal (bottom) meniscus.
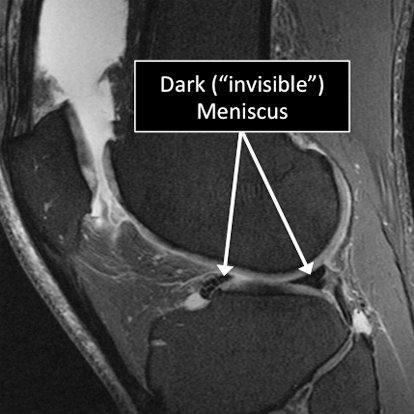
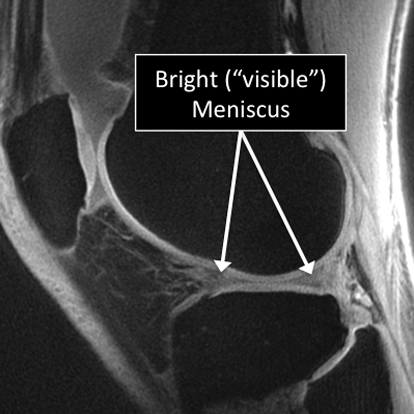
Why Translational MRI of the knee?
-
In the knee, as in many other parts of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
-
There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
-
Some of these “invisible” or dark structures are unique to the knee (knee meniscus) and others are found in other parts of the body (e.g. cartilage, tendons, ligaments, cortical bone).
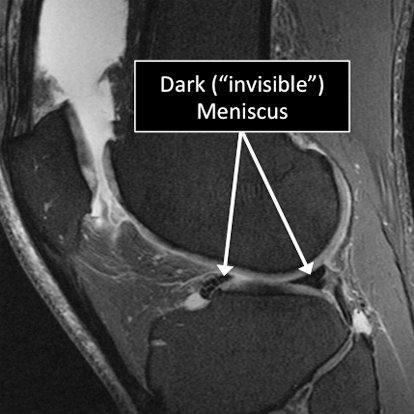
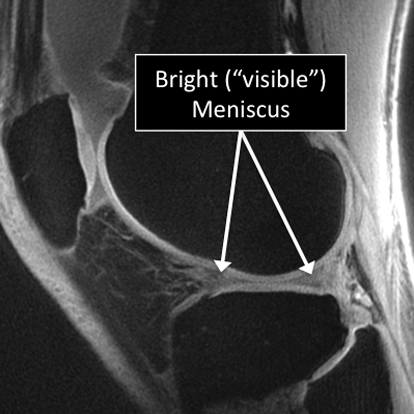
Knee MRI examinations using the standard MRI techniques (top) and translational MRI techniques (bottom).
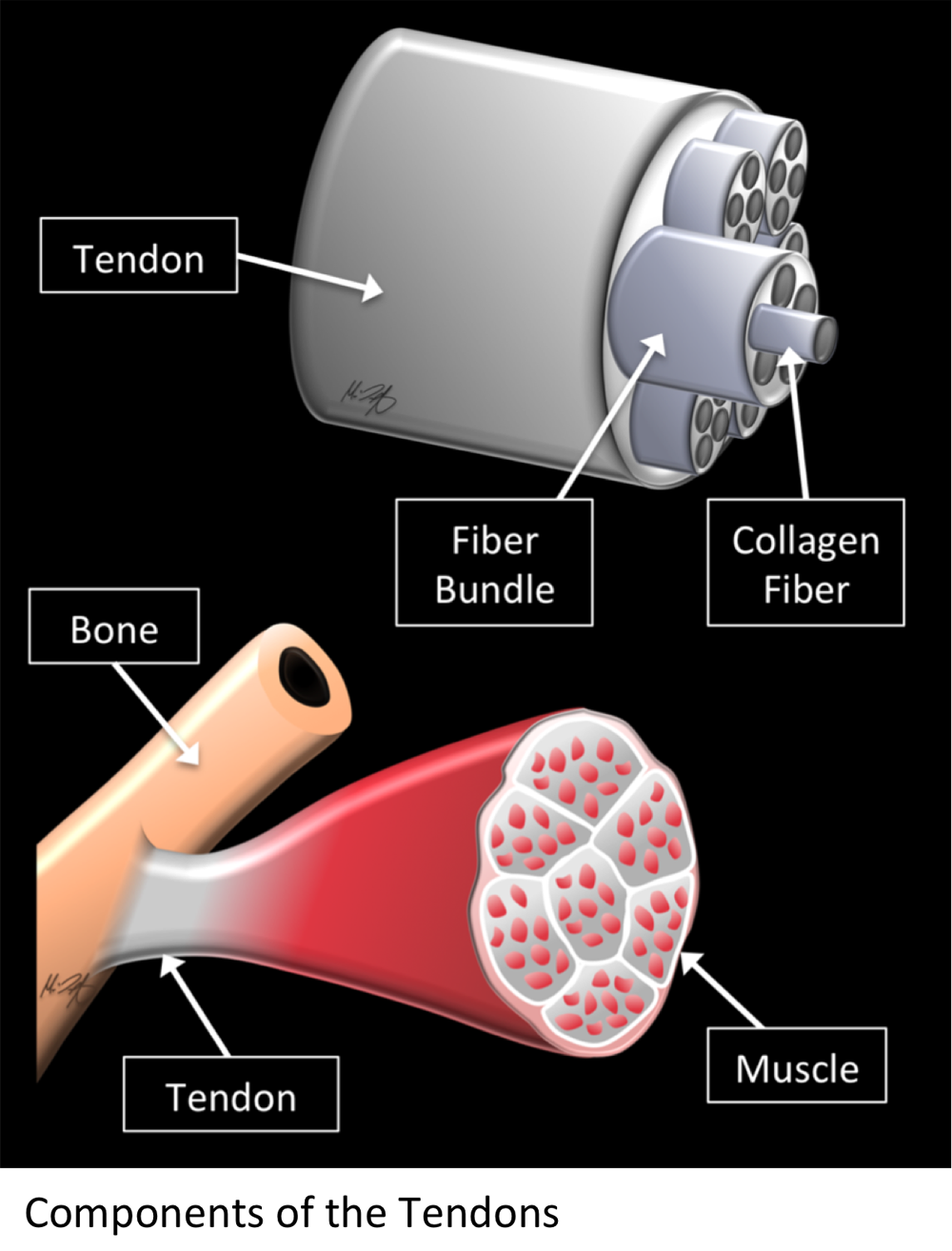
About MRI evaluation of the tendon
-
Specific tendons will be assessed when evaluating a MRI of a specific body region.
-
For MRI of the musculoskeletal system generally there is no special preparation needed unless you doctor specifically requests it.
-
The position of the patient in the MRI machine or scanner will depend on the region of the body to be imaged.
-
The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
-
A piece of plastic, called a “coil”, may be placed on the region to be imaged. This helps to get better quality pictures.
-
The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
What is MRI used for in the tendon ?
-
MRI allows us to see the structure of the tendon.
-
Several injuries or diseases affecting the tendon can be diagnosed using MRI.
-
Common things affecting the tendons include degenerative or traumatic tears, abnormal calcium deposition in the tendons or adjacent to them, tendon degeneration, ganglion cysts (abnormal collections of fluid) in or adjacent to tendons, among others.
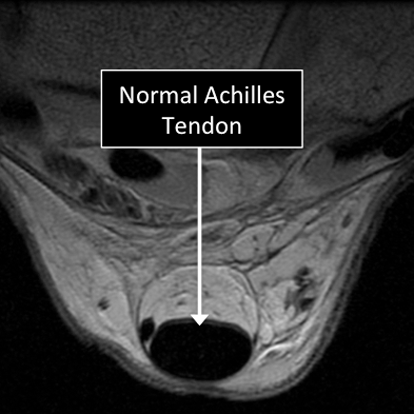
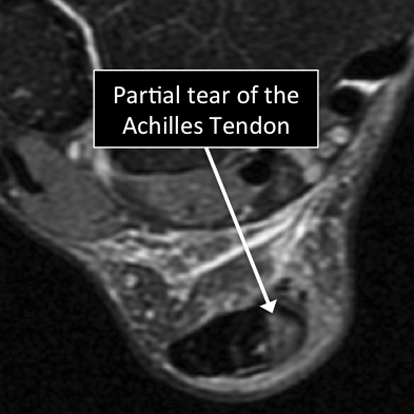
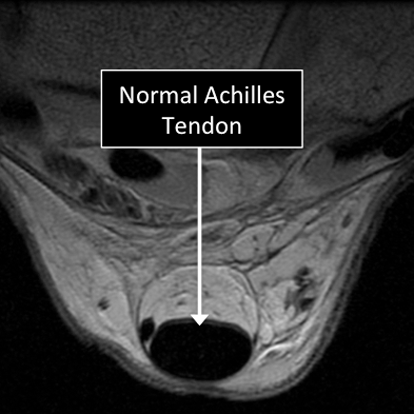
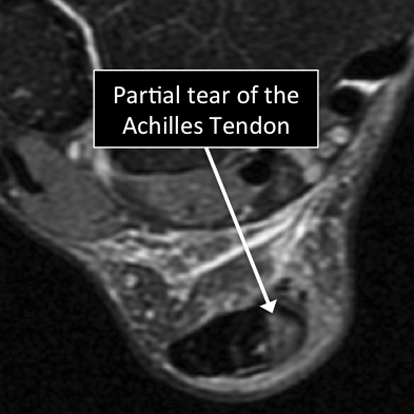
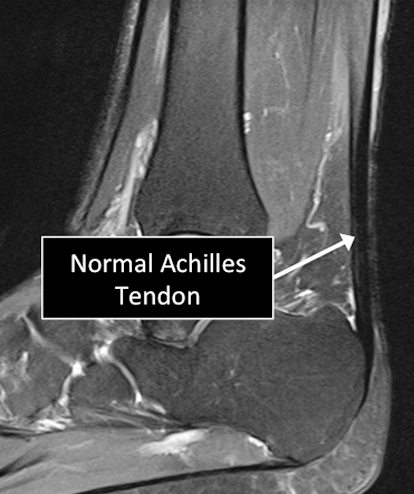
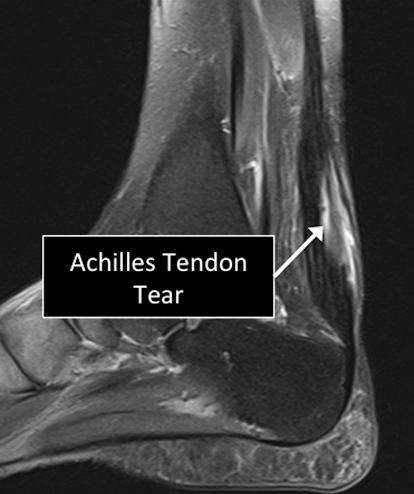
Ankle MRI examinations showing normal (top) and abnormal (bottom) Achilles tendon.
Why Translational MRI of the cartilage?
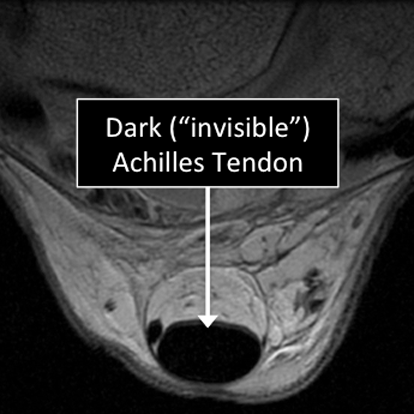
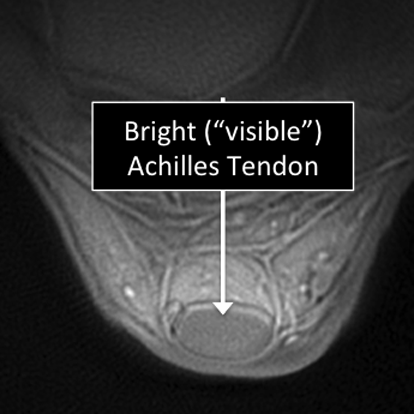
- Tendons are one of the several structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
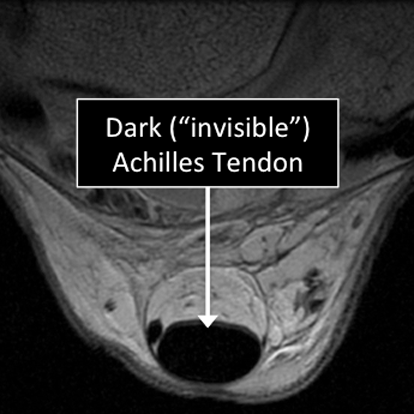
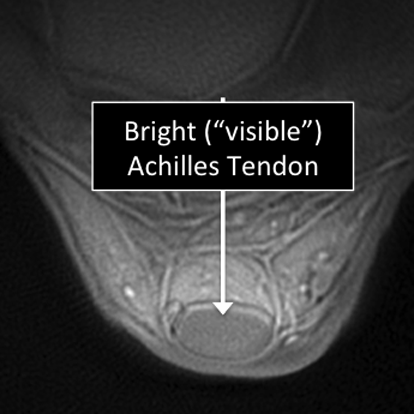
Ankle MRI examinations using the standard MRI techniques (top) and translational MRI techniques (bottom).
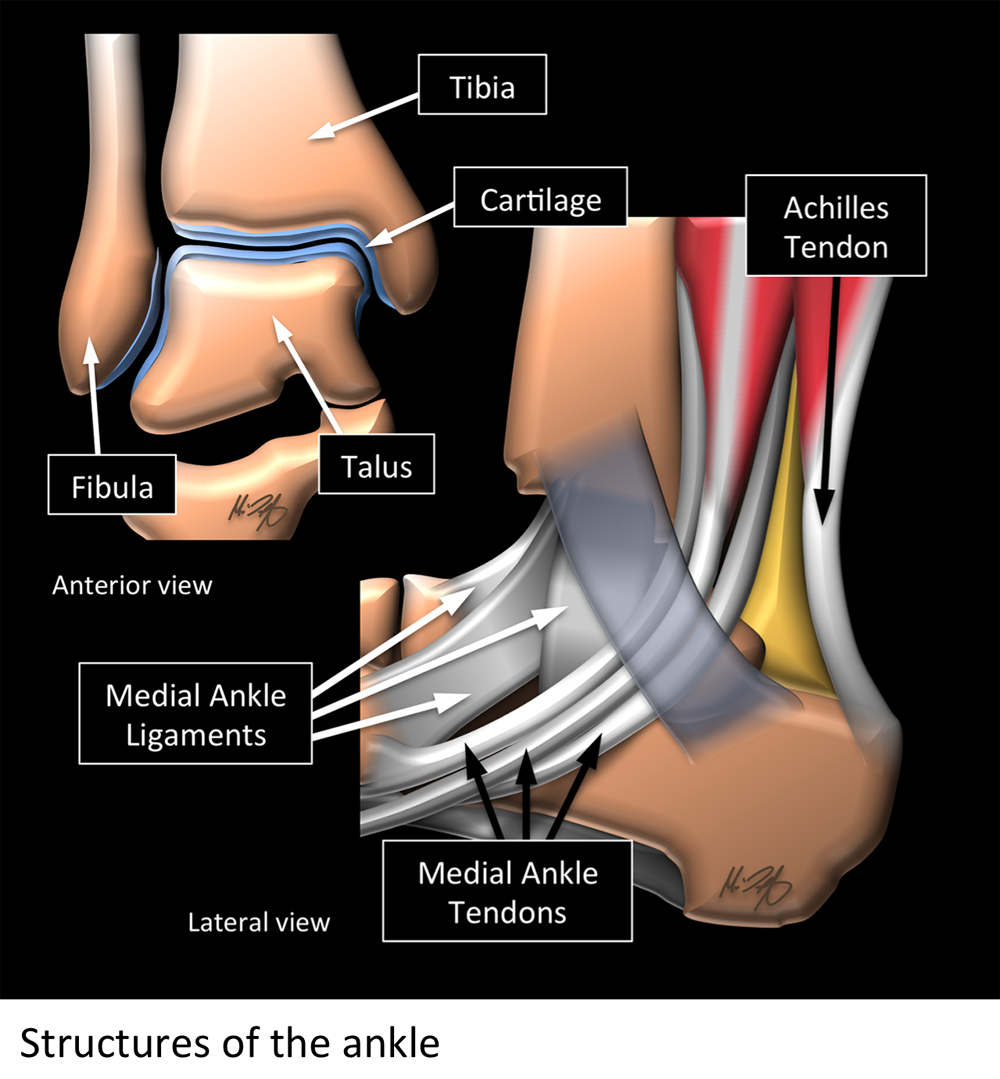
About the ankle MRI
- For ankle MRI there is no special preparation needed unless your doctor specifically requests it.
- The patient is positioned laying on their back inside the MRI machine or scanner with the foot at right angles to the lower leg.
- For ankle MRI there is no special preparation needed unless your doctor specifically requests it.
- The patient is positioned laying on their back inside the MRI machine or scanner with the foot at right angles to the lower leg.
- The patient will be asked to use earplugs as the scanner may produce loud sounds that are normal and will not harm the patient.
- A piece of plastic, called a “coil”, may be placed on the ankle. This helps to maintain optimal position and get better quality pictures.
- The technician will be giving the instructions through a speaker and will check that the patient is comfortable during the examination.
What is MRI used for in the ankle ?
- MRI allows us to see many of the different structures in the ankle.
- Several injuries or diseases affecting those structures can be diagnosed using MRI.
- Common things include degeneration, partial or complete tears of ligaments and/or tendons, damage to the cartilage and/or underlying bone, osteoarthritis, tumors, fractures, among others.
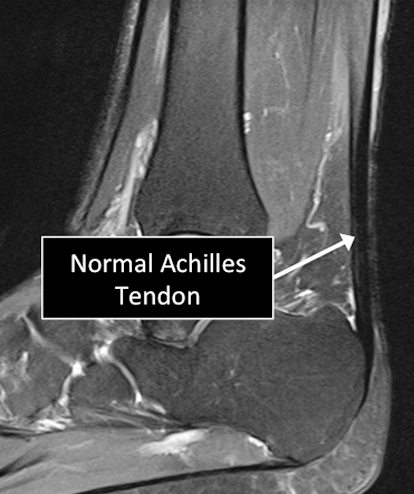
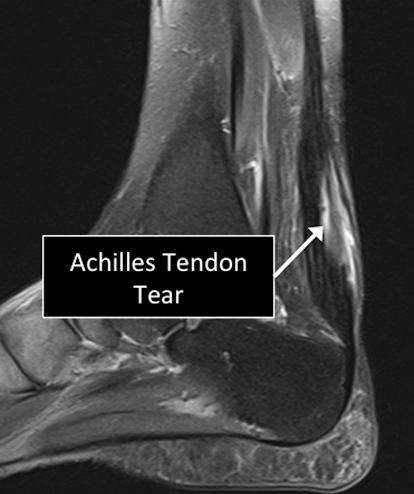
Ankle MRI examinations showing normal (top) and abnormal (bottom) Achilles tendon.
Why Translational MRI of the ankle?
- In the ankle, as in many other parts of the body there are certain structures that can’t be seen (they look black or dark) with the standard MRI.
- There are new “software” programs that allow us to see structures with different contrast (bright versus dark).
- Some of these “invisible” or dark structures are unique to the ankle (e.g. the Achilles tendon) and others are found in other parts of the body (e.g. cartilage, ligaments, other tendons, cortical bone).

.png)
.png)
.png)